Smriti Mallapaty
It was the news Sophie Gryseels had been dreading for months. Almost a year into the pandemic, a seemingly healthy wild mink tested positive for SARS-CoV-2 in Utah. No free-roaming animal was known to have caught the virus before, although researchers had been watching for this closely. “It’s happened,” wrote Gryseels, an evolutionary biologist at the University of Antwerp, Belgium, in an e-mail to her colleagues.
Ever since the coronavirus started spreading around the world, scientists have worried that it could leap from people into wild animals. If so, it might lurk in various species, possibly mutate and then resurge in humans even after the pandemic has subsided.
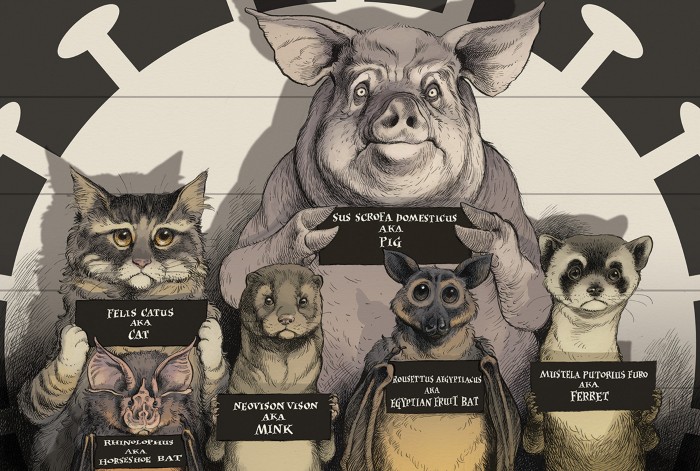
That would bring the tale of SARS-CoV-2 full circle, because wild animals probably brought it to humans in the first place. Strong evidence suggests that the virus originated in horseshoe bats (Rhinolophus spp.), possibly hitching a ride on other animals before infecting people1. In the current stage of the pandemic, with hundreds of thousands of confirmed COVID-19 infections every day, people are still driving transmission of SARS-CoV-2. But years from now, when community spread has been suppressed, a reservoir of SARS-CoV-2 in free-roaming animals could become a recalcitrant source of new flare-ups.
Wild animals are not the only ones to have drawn scrutiny. Studies have shown that SARS-CoV-2 can infect many domesticated and captive creatures, from cats and dogs, to pumas, gorillas and snow leopards in zoos, and farmed mink. Outbreaks in mink farms have already shown that infected animals can pass the virus back to humans.

The first case of SARS-CoV-2 in a wild animal was in a seemingly healthy wild American mink in Utah.Credit: Sven Zacek/NPL
Although these cases have raised concerns, researchers are less worried about viral outbreaks in domestic and farmed animals because such eruptions can be kept in check through quarantining, vaccination and culling. If the virus spreads in wild animals, however, it will be much more difficult to control. “Then there is no hope for eradication,” says Gryseels.
In theory, the virus could evolve as it circulates among animals — possibly in ways that threaten the efficacy of vaccines or make the pathogen more deadly and infectious to people, says Arinjay Banerjee, a coronavirus researcher at McMaster University in Hamilton, Canada. “Not to sound any alarms, but everything we don’t want to see with this virus seems to happen,” he says.
Over the past year, scientists have tried to ascertain how credible and grave the risks are. Global efforts are under way to survey wildlife and catch spillovers as soon as possible. Researchers are testing animals from homes, zoos, shelters, veterinary clinics, farms and their surroundings. If any positive cases are detected, countries immediately notify the World Organisation for Animal Health (OIE), based in Paris. Scientists have used computational models and studied cells and whole animals to identify the species most vulnerable to infection with SARS-CoV-2.
In one year, scientists have collected as much data about the susceptibility of different species to SARS-CoV-2 as was accumulated over the past 50 years for influenza, says Martin Beer, a virologist at the Federal Research Institute for Animal Health in Greifswald, Germany.
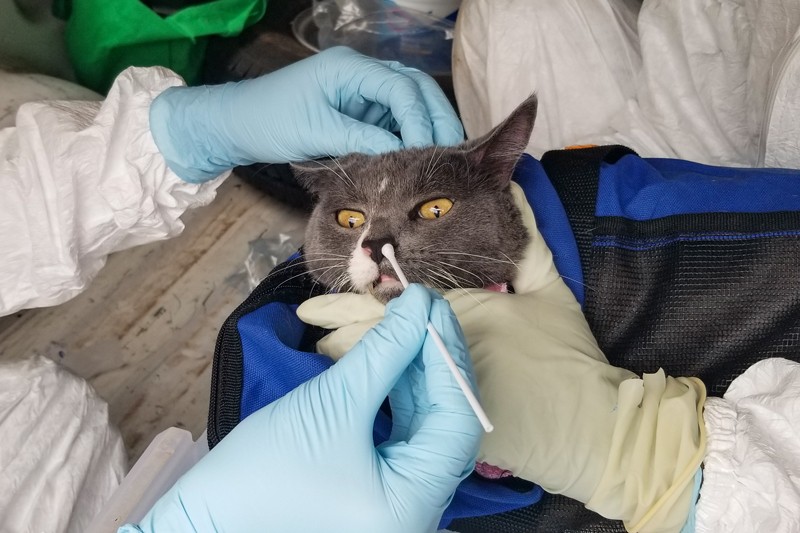
A cat is swabbed as part of a Texas A&M University study of SARS-CoV-2 infection in pets.Credit: Lisa Auckland
Animal infections are rare, and some researchers are reassured by the data collected so far. But others are more cautious. SARS-CoV-2 is known to infect a wide range of animal species (see ‘Animal outbreaks’). This fact, says Gryseels, combined with the large number of infected people, means that, in principle, the virus has had millions of opportunities to jump from people to animals.
Many of those jumps could be passing under the radar. Wildlife studies are difficult to do, and animal infections have not been a priority for much of the research community. The wild mink that tested positive in Utah “could just be the tip of the iceberg”, says Sarah Hamer, an epidemiologist and veterinarian at Texas A&M University in College Station. “The more we look, the more we might find.”
Primary suspects
Early in the pandemic, pigs were top of the watchlist. They are known to incubate other viruses, such as influenza, and they live in huge numbers in close proximity to humans — some 300 million pigs are farmed in China, where the pandemic began. “We are always afraid if pigs are involved,” says Beer.
Pigs can also host coronaviruses. In 2018, researchers described a new bat coronavirus that had killed some 25,000 pigs in southern China2. And in February 2020, scientists working on SARS-CoV-2 showed that it could enter pig cells through the ACE2 protein — the same receptor that it uses to infect people3.
But when researchers began artificially infecting pigs and piglets with SARS-CoV-2, they found that it did not replicate well4,5. These studies suggest that pigs are largely resistant to infection with the virus. “Thank goodness, because with the volume of pig production globally, that would have been a huge problem,” says Peter Daszak, president of the non-profit research organization Ecohealth Alliance in New York City.
With pigs off the priority list, bats became the centre of attention. They are the purported source of SARS-CoV-2, and researchers worried that the virus could spread into new bat populations. In April, the US Fish and Wildlife Service advised scientists to suspend all research that involved capturing and hand-ling bats.
As with pigs, however, the results of studies into bats have been generally reassuring. A study of ACE2 receptors in the cells of 46 bat species found that the majority were poor hosts6. But controlled experiments have shown that some species, such as fruit bats (Rousettus aegyptiacus), can get infected and spread the infection to other bats5. And, with more than 1,400 species, “bats are more of a black box than other animals”, says Gryseels.

Researchers collect bats caught in a cave in Gabon. Bats are suspected of being the source of many human epidemics.Credit: Steeve Jordan/AFP/Getty
Because bats and humans aren’t often in close contact, it’s highly unlikely that people will spread the virus to colonies that haven’t been exposed, says Kaitlin Sawatzki, a virologist at Tufts University in Boston, Massachusetts.
She and her colleagues have tested 321 bats captured from across the northeastern United States and have detected no SARS-CoV-2 viral RNA so far. Scientists say that risk could increase when the pandemic eases and travel and tourism ramp up, along with research and conservation work.
Pet peeves
As the pandemic escalated in 2020, researchers began turning their attention to other animals that are genetically closely related to people, live in close contact with people or are known sources of other viral outbreaks. Laboratory experiments have ruled out a horde of potential hosts — bank voles (Myodes glareolus)7 and raccoons8, for example, and important livestock such as cows9, ducks and chickens4, which all seem resistant to infection.
But the experiments have found many animals that can harbour the virus and pass it on. Among them are ferrets7,9 and cats4, raccoon dogs (Nyctereutes procyonoides)7, white-tailed deer (Odocoileus virginianus)10 and several species of non-human primates10. Infected animals that are sociable — in a herd or with humans — pose a larger risk than lone roamers, says Sawatzki.
Yet even when animals are in very close contact with humans, the barrier to natural infection can be high. In one striking example, Sawatzki tested 29 pet ferrets whose owners had contracted COVID-19. As the owners convalesced at home, tired and feverish, they cuddled, groomed and lounged on their beds with their ferrets, and yet none of their pets tested positive for viral RNA or for antibodies against the infection11. “I could not have been more surprised,” says Sawatzki.
A growing number of real-world studies are beginning to reveal the true risk that animals pose. As more reports surfaced of pets who had caught COVID-19 from their sick owners, researchers took an increased interest in cats, which are often free to slink between households and mingle in the wild. However, their possible role in COVID-19 transmission is a subject of debate.
ANIMAL OUTBREAKS
The World Organisation for Animal Health (OIE) tracks outbreaks, reported by individual countries, of SARS-CoV-2 in animals. An outbreak consists of one or more cases, identified by the presence of viral RNA in an animal. Countries had reported 458 outbreaks by 15 February 2021.
In laboratory settings, cats are easily infected and are contagious to other cats4. They also don’t get very sick, which means that detecting infection is tricky12.
But they get over infection quickly, which means that they probably aren’t infectious for long, says Angela Bosco-Lauth, an infectious-disease researcher at Colorado State University in Fort Collins, who has studied the effects of SARS-CoV-2 infection in cats8. “I don’t think cats pose any risk to human health, even in the long term,” she says.
Several surveys reveal low rates of infection in cats, and no cats have been reported to have passed the infection on to people in a natural setting. Of 920 blood samples taken from a random collection of cats in Germany between April and September, during the first pandemic wave, Beer and his colleagues found only 6 with antibodies against SARS-CoV-2 — some 0.7% — corresponding to the low rates of infection detected in people13. A study14 in a region of northern Italy that was hit hard by the pandemic found that around 6% of 191 house cats had SARS-CoV-2 antibodies.
“There is no reason to be sensational and to be afraid of cats, but you cannot exclude them as a potential, sporadic source of infection in people,” says Jan Felix Drexler, a virologist at the Charité hospital in Berlin.
Mink mayhem
No amount of lab work or fieldwork, however, could have prepared scientists for what has happened on mink farms, says Linfa Wang, a virologist at Duke–National University of Singapore Medical School. “The virus taught us a lesson with mink. It said, ‘You guys can never catch me.’”
An unusual spike in mink deaths at two farms in the Netherlands — and a strong surveillance system — alerted researchers to the first -outbreaks, in April. By the end of 2020, SARS-CoV-2 had reached 70 Dutch farms, as well as farms in about a dozen other countries, including Denmark, Greece, Canada and the United States.
Sawatzki describes the situation in the farms as the “perfect storm”. Animals susceptible to infection are packed together and are in regular, direct contact with infected farmers. In one Danish farm, for example, some 97% of the tested mink had antibodies against SARS-CoV-2, a jump from 6% only 8 days earlier, says Anette Boklund, an epidemiologist at the University of Copenhagen.
As the virus multiplies in infected hosts, it can mutate slightly, leaving in its genome clues to its past travels. By sequencing these genomes, and tracing interactions between infected people and animals, researchers in the Netherlands confirmed in mid-2020 that two farmworkers had caught COVID-19 from mink15 — the first proof that animals could pass the virus on to people. So far, at least 60 people are suspected to have caught the virus from mink, says Wim van der Poel, a virologist at Wageningen University & Research in Lelystad, the Netherlands.
Some researchers worry that, over time, minor genomic tweaks in hundreds or thousands, if not millions, of mink, could eventually add up to changes that make the virus more contagious or more deadly in people, or able to evade treatments and vaccines. In November, researchers in Denmark isolated from mink several variants, one of which, in preliminary cell experiments, evaded antibodies from some people who had recovered from COVID-19. But this variant had been detected in only 12 people and not since mid-September, suggesting that none of those people had passed it on.
A few weeks later, on 1 October, researchers at the US Department of Agriculture captured the wild mink that tested positive in Utah.
Marion Koopmans, who studies virology at the Erasmus University Medical Centre in Rotterdam, the Netherlands, says she was not surprised that a wild mink had contracted the virus, given the high levels of contamination observed in bedding and dust around affected Dutch farms, and that mink sometimes escape from farms and establish themselves in the wild. More than a dozen mink — caught in the wild but probably escapees from farms with active outbreaks — have tested positive for SARS-CoV-2 viral RNA or antibodies in the United States and the Netherlands.
So far, the mink captured in Utah is the only wild animal to have tested positive, but several national and regional research consortia are continuing to survey wild animals near mink farms for evidence of infection.
Some countries have taken sweeping measures to prevent the virus spreading in mink. Denmark — the world’s largest producer of mink skins — and the Netherlands have culled their entire mink populations, totalling nearly 20 million animals. Other countries are considering vaccinating their mink. The pandemic is “speeding up the end of mink farming”, says Drexler.
The story of mink and COVID-19 has confirmed researchers’ early fears that the virus can find refuge in animals in ways that are difficult to predict and control, and that it can then jump back to people. But it remains unknown whether SARS-CoV-2 can spread efficiently among wild populations, says Koopmans, who is monitoring wild mink in the Netherlands. “Mink are rather solitary animals when left alone, so that may work to our advantage,” she says.
Scientists also wonder what is happening in China regarding mink and other animals farmed for fur, such as the raccoon dog — a fox-like animal that some researchers think could have been an intermediate host of SARS16. Very little research on SARS-CoV-2 and animals has been published from China, although a World Health Organization (WHO) team investigating the origins of SARS-CoV-2 said at a press briefing on 9 February that results from testing wild and farmed animals across China had found no evidence of the virus circulating in these animals.
Surveillance efforts are becoming more unified. The OIE, the WHO and the US Centers for Disease Control and Prevention have all published guidance on surveying animals (none recommends widespread testing, but the WHO advocates testing around infected fur farms). The OIE meets monthly with researchers in the field to discuss the latest research on animals in the pandemic.
No comments:
Post a Comment