WILLIAM A. HASELTINE

BOSTON – The United States has now entered its fifth wave of COVID-19 infections. In each one, the country has paid a high price for doing far less than it could. In the first wave, lockdowns and other restrictions were spotty. Then came untested and unproven treatments. With the vaccine rollout, new infections were pushed down substantially, but now the Delta variant has started pushing them back up in unvaccinated populations.
At each stage, the SARS-CoV-2 virus that causes COVID-19 was underestimated. From what we know of its ability to adapt and thrive through random mutations, there is only one viable option for long-term disease control: a strategy that combines a rapidly growing arsenal of vaccines and antiviral drugs with strong public-health measures and deeper global cooperation.
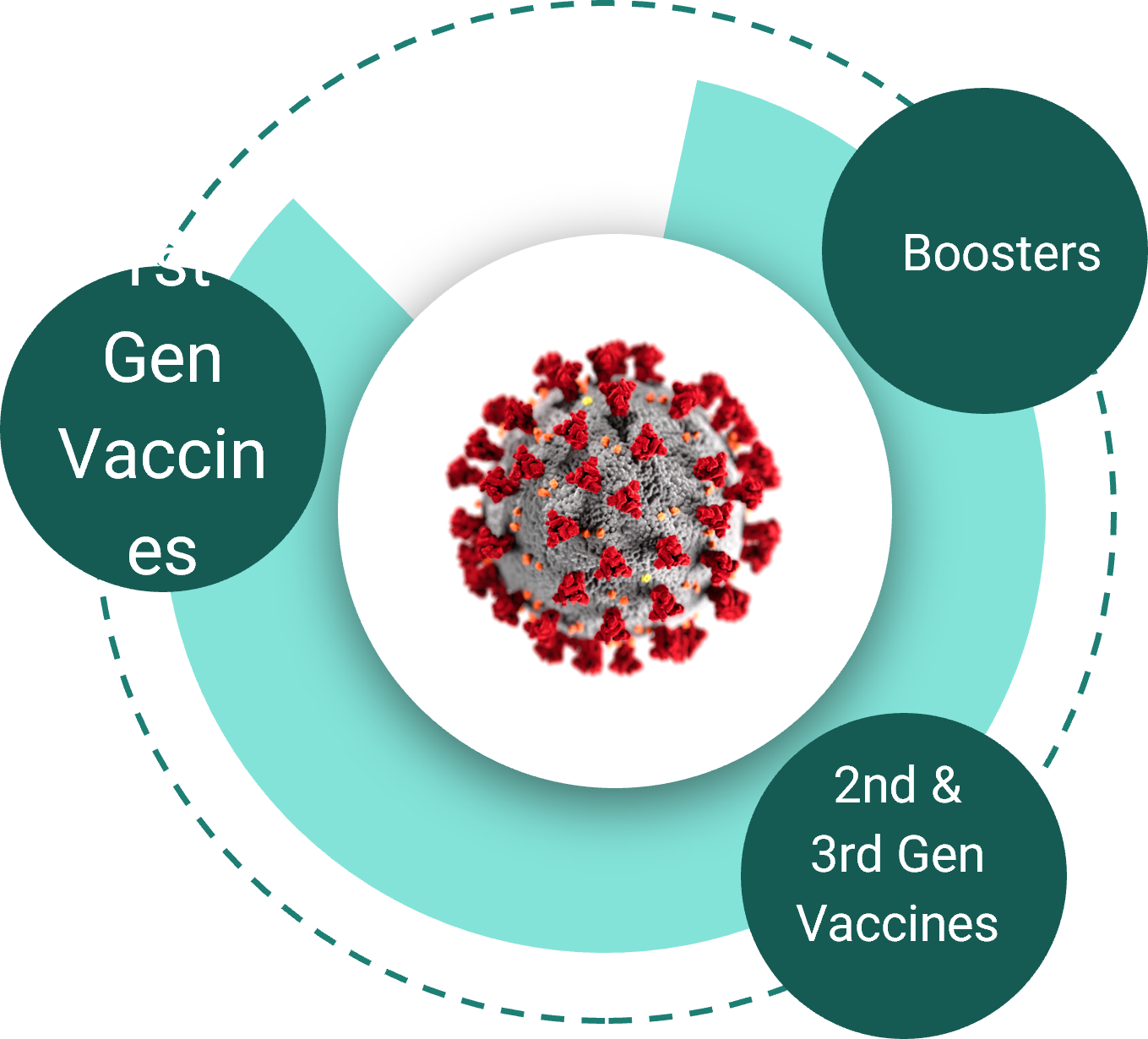
Vaccines comprise the first ring of defense against COVID-19. The first generation of vaccines in the US are highly effective, and the second, third, and subsequent generations will be even stronger. But even with booster shots in hand and next-generation vaccines tailored to new variants, vaccination alone is unlikely to end the pandemic.
Vaccines won’t work for everybody. In the best-case scenario, against the original wild-type virus, vaccines still fail about 5% of the time. And the Delta variant has proven more adept than previous strains at breaking through vaccine protections. Even if the entire US population was vaccinated, 17.5 million Americans would still be at risk of infection and disease if exposed to the virus.
Moreover, there are substantial populations of people with underlying conditions that diminish vaccine efficacy; these include organ-transplant recipients, people taking immunosuppressant drugs, cancer patients, and a fraction of the elderly population. And like the protection offered by the annual influenza vaccine, early evidence suggests that vaccine-induced immunity against COVID-19 may fade over time.
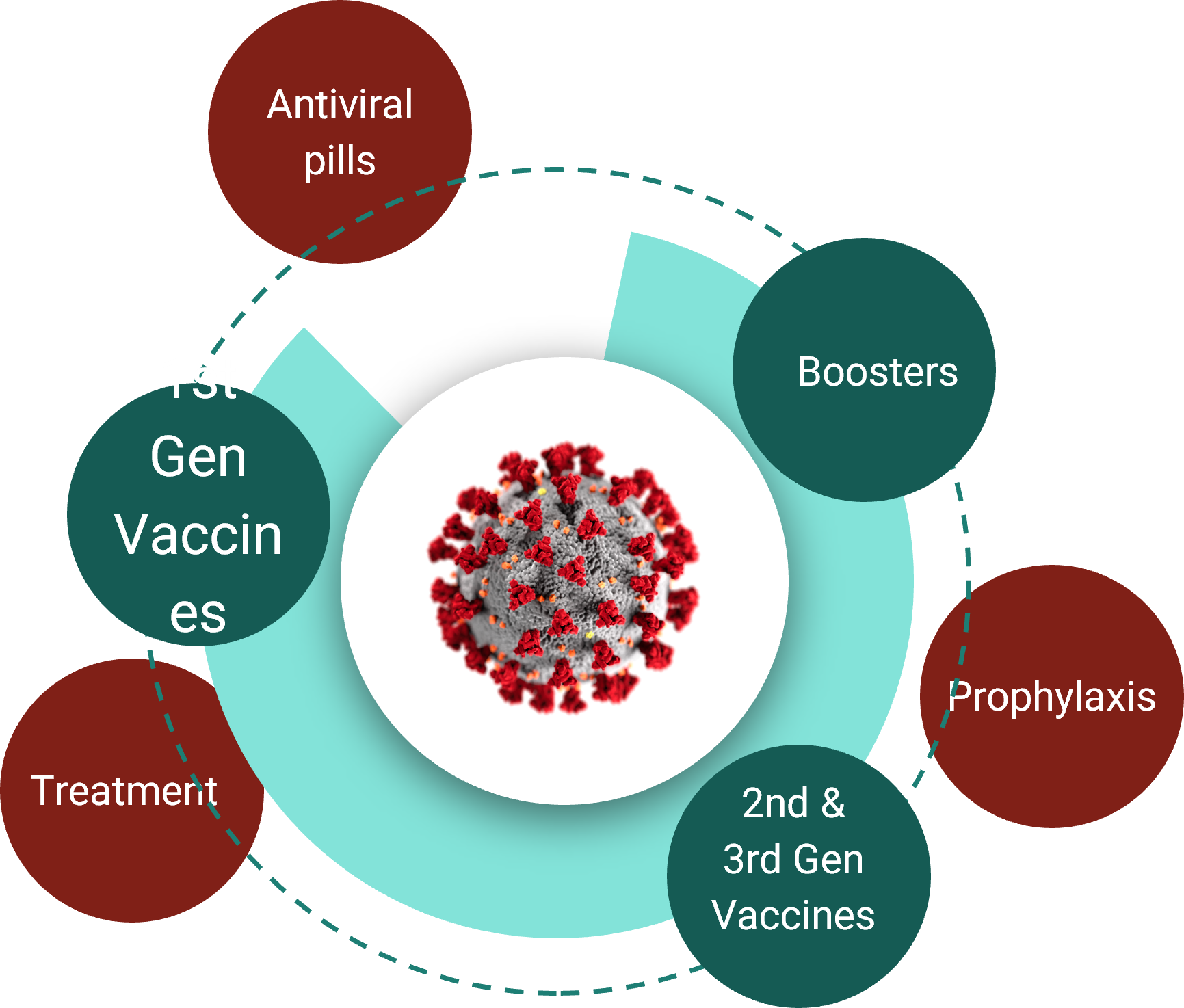
Antiviral drugs and prophylactics will be needed to fill the gaps and provide a second ring of defense. The US government recently committed $3.2 billion to develop antiviral therapies for COVID-19. While most of the focus has been on using these drugs as a treatment, their true potential lies in pandemic control, because administering prophylactically can prevent people who have been exposed to the virus from becoming ill or passing on an infection.
True, the current generation of these drugs cannot be used widely, owing to their high production costs and the need for intravenous infusions in a clinical setting. Nonetheless, we have achieved proof of principle. Ideally, the next generation of antivirals will come in pill form, giving them enormous potential for use in high-risk settings such as long-term care homes, where there are many immunosuppressed individuals who cannot rely on vaccines for protection. The same approach applies to schools, businesses, professional sports teams, and even ships at sea. If one person tests positive for COVID-19, everyone around him could take a pill to help stave off infection.
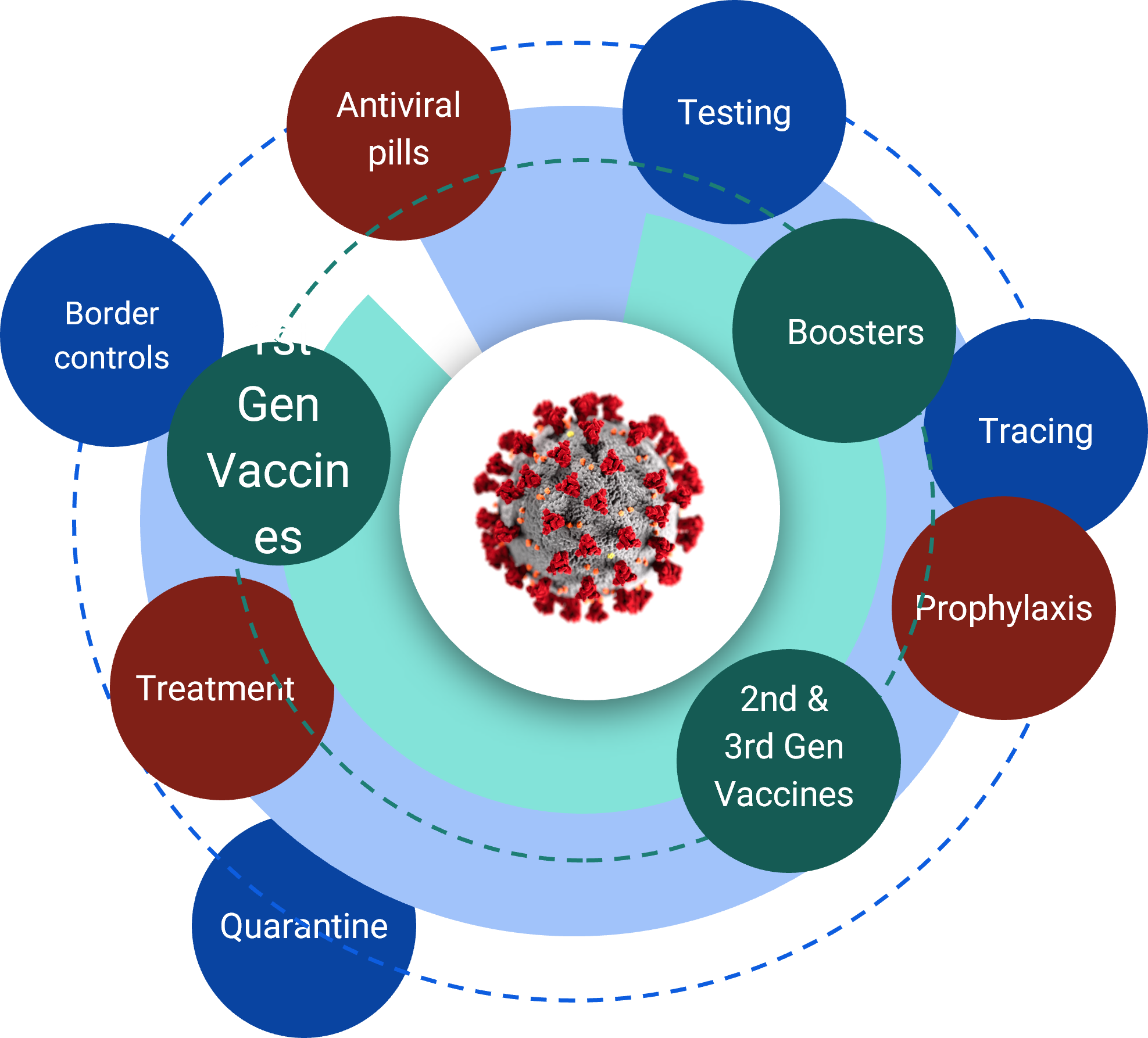
The next ring of defense will come from public-health measures to contain the spread of the virus. Countries such as Australia, China, New Zealand, Singapore, and Taiwan have made effective use of widespread testing, exhaustive contact tracing, mandatory isolation, tight border controls, and quarantines for new arrivals. Such strategies have been critical methods of protection in the face of nearly every infectious disease in recent history. But in the US and other countries around the world, testing and contact tracing have stalled (or never got off the ground in the first place).
Fortunately, new antiviral prophylactic drugs can help make up for some of these failures. As opposed to “test, trace, and quarantine,” the mantra may become “test, trace, and swallow a pill” – a much more attractive alternative. These drugs also may help open new opportunities for travel, eliminating the need for long quarantines.
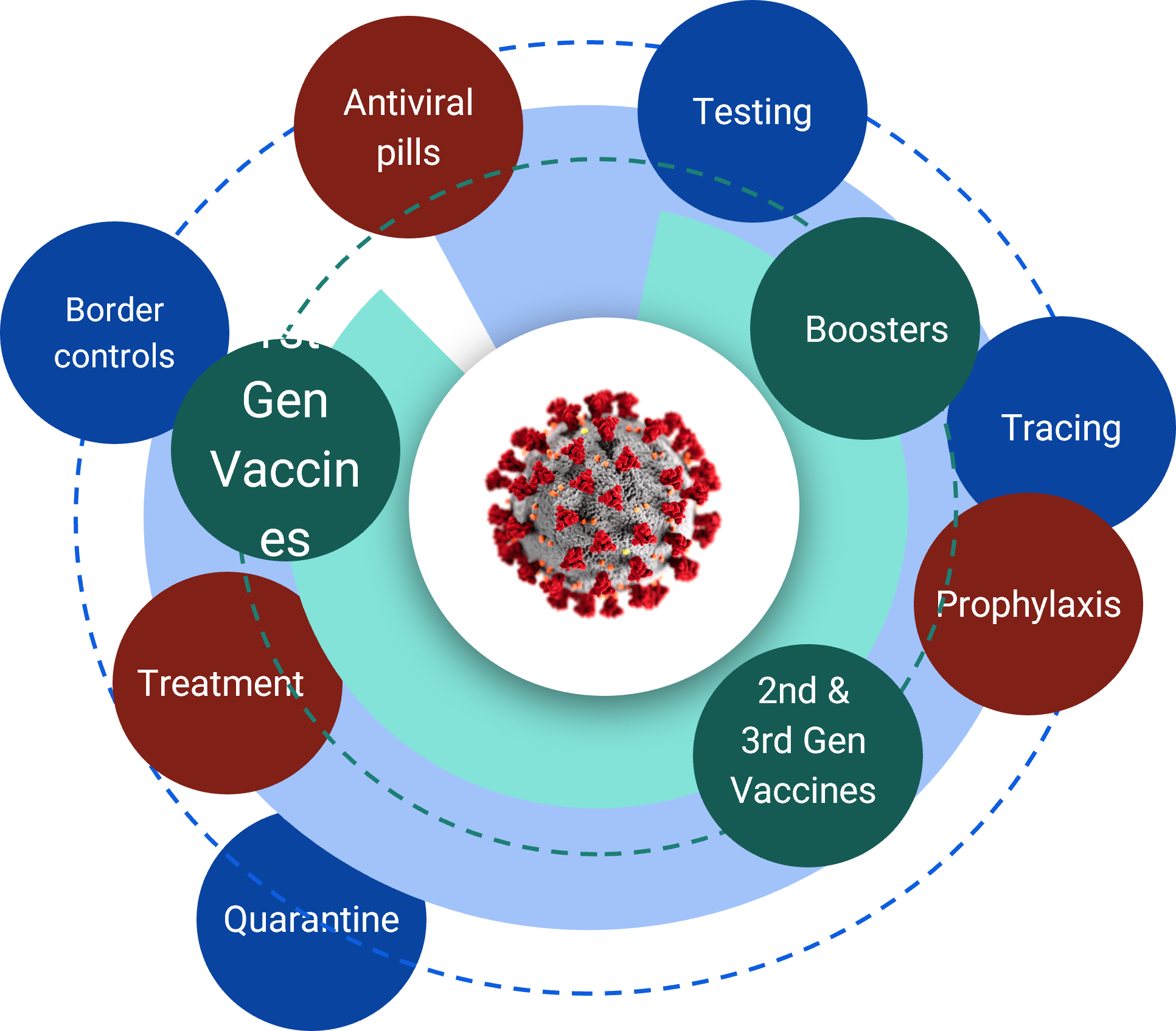
The first three rings of protection form an excellent defense. But they will be insufficient unless they are implemented everywhere. To provide the final ring of protection, the international community must work together to improve disease surveillance, and to provide universal access to tests, treatments, and vaccines.
Here, the Access to COVID-19 Tools (ACT) Accelerator and its vaccines pillar, COVAX, were an important first step. But the power of the platform has been diminished by self-interest and vaccine nationalism. Still, there is hope for the future now that many high-income countries have a surplus of vaccines. There are also efforts underway to increase local vaccine production in underserved areas.
In addition to these efforts, the international community needs to invest in global disease surveillance to identify new outbreaks, especially ones caused by highly infectious variants that can quickly take hold and spread. This requires an enhanced surveillance presence, increased sequencing of the virus across all communities, and a near-real-time method of sharing the data broadly.
With the proper frontline mechanisms in place, the global community of scientists, researchers, and pharmaceutical manufacturers will have to determine how vaccines and treatments fare against each new variant, and what can be done to mitigate their spread and reduce their likelihood of emerging.
Eighteen months into this pandemic, we have what we need to end it. Now, we must apply our knowledge and tools. No single approach will ever be enough. But, together, the four defensive rings – vaccines, antivirals, public-health measures, and international cooperation – can help us eliminate COVID-19 as a life-threatening disease and allow for the dawn of a better life than the one we left behind.
No comments:
Post a Comment